A 26-year-old male health-care professional presented to the sports medicine department with right-sided distal medial thigh and knee pain after exercising. There was swelling of the medial side of the knee and pain with extreme flexion. Radiographs were interpreted as a suprapatellar joint effusion but, in retrospect, demonstrated a lytic lesion in the superomedial aspect of the distal part of the femur. The patient was diagnosed with anterior knee pain and was treated conservatively. He returned 4 weeks later, with partial improvement but persistence of pain, worse with prolonged standing. There were no systemic symptoms. Examination demonstrated improved swelling and knee motion. Radiographs (Fig. 1) demonstrated a lytic lesion superomedially in the distal part of the femur, with a surrounding border and associated joint effusion. A stress fracture was diagnosed because of a history of running, activity-related pain, and some improvement with activity modifications. Due to partial improvement, no further imaging was obtained, and the patient was prescribed physical therapy.

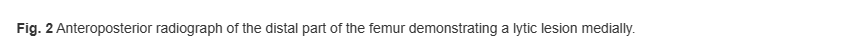
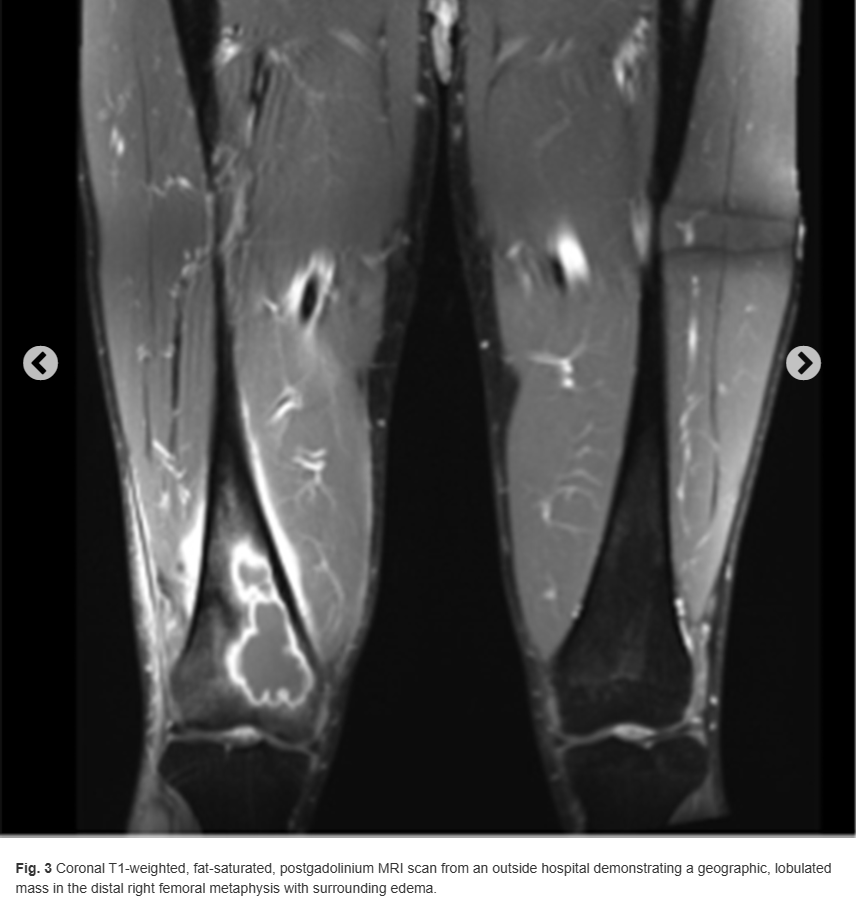
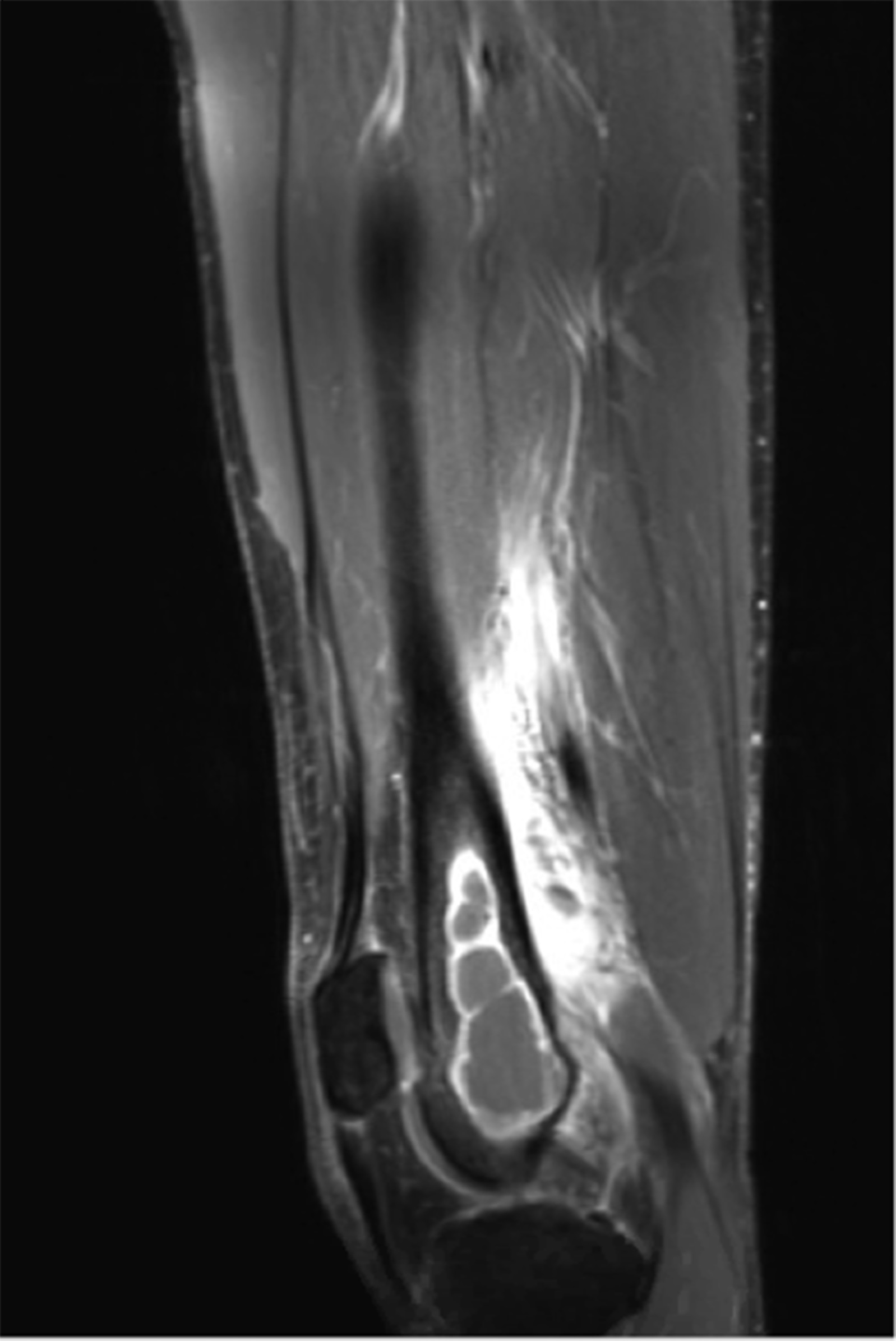
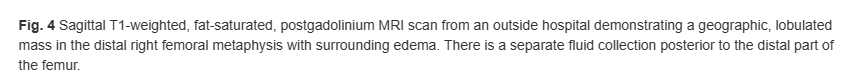
Six months later, the patient returned with continued pain. Radiographs demonstrated a cystic bone lesion (Fig. 2). A magnetic resonance imaging (MRI) scan showed an 8-cm sharply marginated, lobulated mass in the distal right femoral metaphysis, surrounding edema, and a heterogenous fluid collection in the soft tissue posterior to and communicating with the lesion (Figs. 3 and 4). The differential diagnosis included neoplastic processes, such as telangiectatic osteosarcoma, aneurysmal bone cyst, or an atypical giant cell tumor.

At the patient’s orthopaedic visit, the only notable finding was tenderness with palpation medially and posteriorly about the thigh. He had full motion of the knee and was able to ambulate without pain.
Computed tomography (CT)-guided intraosseous and soft-tissue core needle biopsies were performed posteromedially, which demonstrated benign inflammatory tissue, but was nondiagnostic because necrotic tissue was identified. Culture samples were not obtained, and blood was not drawn to determine erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels.
Subsequently, an open incisional bony biopsy was performed through an anteromedial approach. An incision was made over the vastus medialis oblique (VMO). The VMO was split, and subperiosteal dissection was performed to allow for a bony window. Curettes were used to remove intraosseous necrotic tissue. A frozen section showed necrotic tissue. One set of culture samples was obtained. The bony window was replaced, and the incision was irrigated and closed. The patient was instructed to not bear weight.
The pathology of permanent sections demonstrated necrotizing granulomatous inflammation. Stains for bacterial, fungal organisms, acid-fast bacilli, and intraoperative aerobic and anaerobic cultures were negative. An infectious disease consultation was obtained. The patient had previously tested negative for tuberculosis and had no known exposures. Further workup, including a chest radiograph, Bartonella and fungal antibody panels, complete blood count, acid-fast bacilli blood culture, and QuantiFERON Gold were negative. Due to uncertain etiology and negative culture and stains, no antimicrobials were prescribed. The sample was sent for mycobacterial and bacterial (16s) polymerase chain reaction (PCR) analysis. No mycobacterial or other bacterial DNA was detected. The plan was to follow his examination and acquire an MRI scan in the future. Return to activity was tolerated well. Radiographs at 1 month (Figs. 5 and 6) and 3 months (Fig. 7) demonstrated a healing cavitary lesion of the medial femoral condyle without any interval progression of the lesion. An MRI scan was not acquired because of clinical improvement.



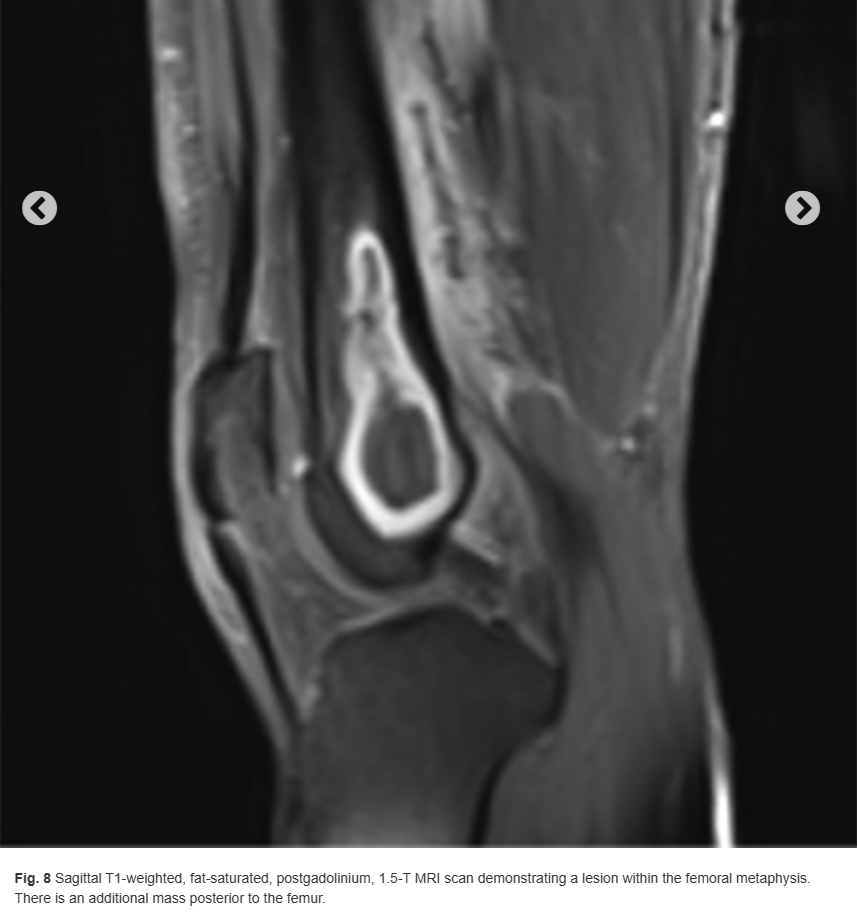
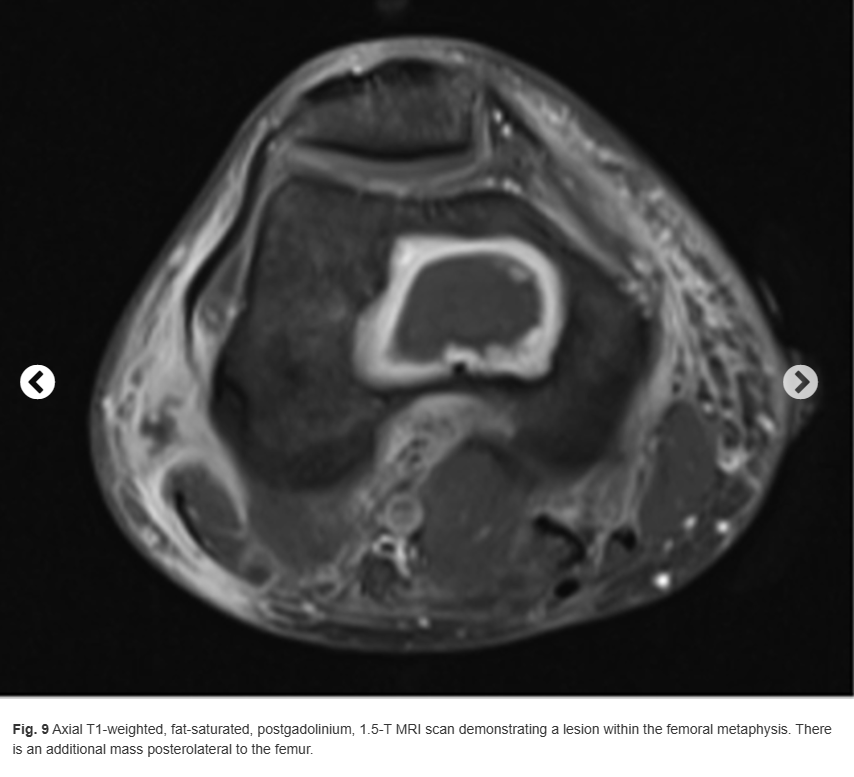
Two months later, the patient’s distal thigh became swollen with associated fevers, chills, and night sweats. The site became indurated, warm, and tender. He presented to the emergency department where fluid was aspirated with a purulent appearance and sent for culture. The blood cultures were negative. The CRP was 60.8 mg/L (reference range, 0.0 to 6.0 mg/L), and the ESR was 8 mm/h (reference range, 0 to 10 mm/h). The patient’s peripheral white blood cell count had increased from 5,300 cells/μL at the time of his infectious disease consultation to 12,400 cells/μL during this presentation. Due to the abovementioned findings, an MRI scan was acquired, which demonstrated a lesion within the distal femoral metaphysis (Figs. 8 and 9).